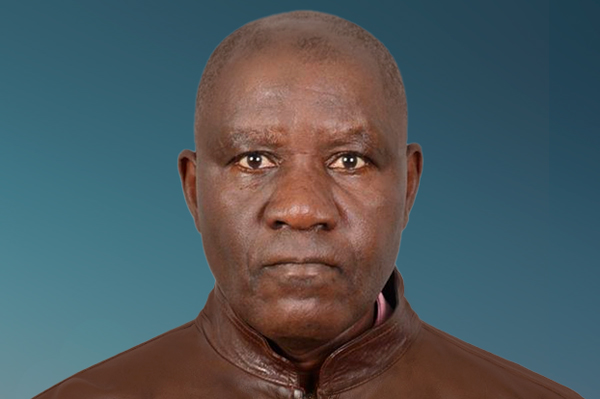
I am Tendai Moyo, a Zimbabwean advocate, founder of Brave Little Hearts Zimbabwe. After losing my infant daughter to a treatable heart disease condition, I also live with multiple NCDs while caring for my 12 year old daughter with fibromyalgia.
I advocate for children with childhood heart disease and rare NCDs. As a member of the World Heart Federation, ex-board member of Global Arch, and NCDI Poverty Network member, I push for improved healthcare access, awareness, and policy change.
15 July 2025
Grieving and standing in the eye of broken healthcare
My name is Tendai Moyo, and this is the first episode of my NCD Diaries. In this episode, I talk about my lived experience with various NCDs both as a caregiver and as an affected individual. From childhood, I cared for my parents with asthma, diabetes, and hypertension. Today, I live with multiple NCDs, including stroke and arthritis, while also caring for my daughter who has fibromyalgia. I share the heartbreaking loss of my infant daughter due to a complex heart condition, misdiagnosis, and systemic neglect.
Transcript
My name is Tendai Moyo, and welcome to the first episode of my NCD Diaries. In this episode I will talk about my lived experience with various NCDs both as a caregiver and as an affected individual.
I live in Zimbabwe with my three children, having lost my fourth-born at ten months of age. I am a young widow living with multiple non-communicable diseases. I have also been a caregiver from a young age to both my late parents who suffered from asthma, diabetes and hypertension and am currently looking after my 12-year-old daughter who lives with fibromyalgia. Her condition brings continuous pain, stigma, and exorbitant out-of-pocket expenses for numerous tests and medications, some of which have caused adverse effects. She faces constant absenteeism from school, insomnia, is in constant pain and has many allergies and intolerances , including weather . These challenges are our everyday reality, alongside the struggle to put food on the table and send my other children to school.
My medical journey has been tough and straining. I live with arthritis from a hip joint injury, eye problems, and I am a stroke survivor. I have also battled depression due to multiple losses in my family — a battle made even more difficult by a healthcare system that has consistently failed to offer support or hope. Thankfully, I have received counselling, which has helped me begin to process some of the deep mental trauma I carry.
My earliest memories with my late daughter are of several hospital admissions, sleeping on cold floors, lacking access to medication, and constantly struggling to get her necessary care. She was diagnosed at six months with tricuspid atresia, a complex heart condition. Tragically, the signs and symptoms were present from birth — cyanosed lips, difficulty in breathing, cold hands and feet — but every time I voiced concerns at our local clinic, they were dismissed. She was a very big baby, so her size was seen as an indication of health. My concerns were attributed to paranoia. Each visit to the hospital was met with a clean bill of health.
At four months, when she was failing to thrive and still weighed 4.5kg — her birth weight — I was told I was not feeding her adequately and instructed to express milk into a cup instead of breastfeeding. Deep down I knew something was wrong. She would sleep for prolonged periods, tire easily when breastfeeding, and regurgitate her milk more than usual. I raised these concerns repeatedly but was told not to compare my children because they grow differently.
Eventually, some people, including family members, began whispering that my daughter’s failure to thrive and reach milestones like crawling and sitting was due to witchcraft. Whenever we went to hospital, the whispers grew louder and I was pressured to seek traditional remedies. Though I didn’t believe in those methods, the pressure became overwhelming. I took my child to a herbal clinic, where I described her symptoms and was given an all-in-one concoction which I was told would heal her (Musimboti). It only worsened her breathing difficulties. This was similar to seeing a repeat of what my mother went through, whose asthma worsened with traditional steaming methods. I threw the concoctions away. But the void of not knowing what was wrong, coupled with our poor financial situation, meant that private care was out of reach and we had to continue relying on public hospitals.
Before her diagnosis, during one of her many admissions there was an early and traumatic incident where we were told to remove her from oxygen and walk to a separate building in the cold for an echocardiogram. I explained that the doctor who attended to her had said she needed continuous oxygen as her saturation was very low but we were told there was no portable option and we had to go to the next block without any oxygen. We arrived to be told to wait in a long queue. She grew pale and cried for some time. I went to the attending nurse and I explained that I could not continue in queue and needed to be attended so that she could be put on oxygen again, but I was ignored. I had to beg fellow patients to let us skip the queue. Once inside, the doctor acted quickly and instructed us to get her back on oxygen immediately.
After her diagnosis, her doctor told us her condition could not be treated in Zimbabwe, hence referred us to a hospital in India for surgery costing $20,000 including flights and accommodation. When we asked for cheaper alternatives, the doctor insisted on the particular hospital she had recommended. The price was too steep for us, so we searched for other options. We made appeals through media and any platform available, and were approached by a local agent from India who said they could offer us a lessor charge. However, they needed our child’s medical report and supporting documentation for the transfer and surgery. The same doctor who attended to us at the public hospital insisted that we go to hospital she recommended. Little did we know that when doctors make a referral they are given commission, so we suffered and were clueless as to why our child's documents were being held for more than six months. Those reports were crucial. Meanwhile, we were charged for expensive review appointments by the same doctor, which felt like exploitation of our desperation.
Eventually, we were referred to another doctor at the public hospital, who said they would see how they could assist with a referral to a hospital in the capital where cardiac specialists were located. The first doctor was said to have gone out of the country and they did not know when she would be back. The next Monday, we were packed and ready for travel and made our way to the hospital to get the referral letter and medical report. We waited all morning for the doctor to arrive. It was exhausting and we were hungry. My breast milk was not coming out that much, we had not anticipated such a long wait. When the doctor arrived after examining her, he said she was very pale and had to admit her and we could not travel. Little did I know that this would be her last admission. We were taken to ICU and she was removed from the portable oxygen we kept on her and was put on the hospital oxygen. We were now purchasing a constant supply of oxygen which was very expensive. But in the hospital where she was admitted, they forgot to put it back for more than three hours after nebulization and we had been asked to go out from her ward as they were attending to one of the children who had collapsed at ICU. We sat outside waiting re- entrance. She was left lying flat, which compromised her breathing. When I pointed this out, the nurses dismissed me. One nurse even handed me an injection and sarcastically said, “You seem to know it all, why don’t you treat your child?”
By the time she was re-connected to oxygen, I was left to more endless waiting. I was then told the sad news that she was on a ventilator and that she was in a very critical condition. We went to see her with all the pipes and tubes on her, but she did not last till morning.
As I later learnt, reporting neglect in hospitals usually leads to withdrawal of service, hence many people suffer poor service in silence. Even after the death of my child, it took more than six months for our grievances to be acknowledged and all we got was an apology for the delay in paperwork and the forgotten oxygen behind closed doors, but nothing was done to those who made us suffer. The negligence we experienced was all swept under the carpet. Grieving families are labelled as emotional and blamed for not understanding losses, but the neglect is real, with no system in place to address these challenges.
The voices of poor communities affected are rarely included in programming, making it difficult to be heard. Healthcare is available to the elite in private hospitals; the poor must bring their own medication, syringes, and bandages to under-resourced government facilities.
The raw pain and trauma of navigating this broken system while living with an NCD, of watching loved ones die unnecessarily, of being silenced, ignored, and blamed, has left deep scars. The mental toll has been immeasurable. For a long time, I lived in despair, helpless and broken. But I am slowly healing, thanks to counselling and support from others who have walked this painful path.
29 August 2025
When silence is no longer an option
In this episode, I share how personal loss and lived experience led me to challenge a broken health system, amplify unheard voices, and fight for children living with heart disease and rare NCDs in Zimbabwe. This is a story of pain, purpose, and pushing forward when the system fails the most vulnerable.
Transcript
In this episode, I will talk about my choice to take the road less travelled: advocacy, especially in a country such as ours where there is great difficulty in speaking out due to fear and hopelessness. I also share the challenges faced by vulnerable communities in everyday life.
After my experience, I founded Brave Little Hearts Zimbabwe, a support organization for parents and caregivers of children and youth with heart disease and rare NCDs.
Our advocacy began from a place of lived experience—navigating a broken health system that lacked diagnostics, specialist care, and essential treatment. We’ve since become a national voice for childhood NCDs, raising awareness, engaging policymakers, and influencing health policy discussions.
The road has been far from easy. In setting up my organisation, and trying to conduct our advocacy efforts, we experienced bureaucracy and socio-economic barriers that can push any advocate to the brink of giving up. But we kept going. For me, the drive to continue went beyond burying my own child and other family members. I was driven by the fight against injustice, trauma, and a petition for the right to health for all.
I think of Tapiwa’s mother, who shared their story: “We travelled over 300km to Mpilo Hospital only to be told the echo machine wasn’t working. They sent us back with nothing. We spent all we had just to get there.”
Or Tanaka’s father, who said: “Doctors told us surgery had to be done outside the country. We don’t even have money for passports, let alone for a visa or hospital bills in India. The government isn’t helping. We are watching our son fade.”
Then there’s Rutendo’s aunt who was left caring for her niece with Triscupid Atresia after her mother died. She has been fundraising for over a year: “It is difficult to get donations, and the delay is worrying because our child is always sick. The Ministry of Health does not fund emergencies such as ours, nor do they offer treatment locally. We were told that our child needs surgery within the first 6 months of life and our child is now one year old.”
Nyasha’s mother broke down and said: “We missed two months of medication because I had to choose between buying her pills or feeding the family. I prayed every night her heart would hold on. This is not neglect—it’s poverty.”
I also share a heartbreaking story of unrecognized NCDs in children, told by my 12-year-old daughter Ropafadzo who lives with multiple autoimmune conditions.
“They say you can’t see pain. I wish that wasn’t true. If people could see what I feel, maybe they’d stop asking, ‘Are you really sick?’ or giving me that look like I’m lazy or just trying to skip school. But I’m not. I miss school. This pain is real and it’s everywhere in my body - chronic migraine, headaches, painful swollen joints, nose bleeds, allergies, weather sensitivity, noise sensitivity, chest pains, heart palpitations, difficulty in breathing.
I went through years of the wrong meds. I did test after test. Blood tests, x-rays, scans, referrals. ‘Everything looks fine,’ they said. But I wasn’t fine. And because they couldn’t see it, some doctors—even some people around me—started saying it was ‘all in my head’.
I want to live. I want to learn. I want to become a general surgeon—the kind of doctor who saves lives and doesn’t brush off pain just because they don’t understand it or see it. Everything is so expensive. The right doctors, therapy, tests, supplements, food that helps—all of it costs too much. It's not fair that getting sick also means going broke.”
When Ropafadzo was diagnosed with multiple autoimmune conditions, it felt like falling into a void. There was no clear diagnosis pathway. No national guidelines. No awareness campaigns. Just confusion, silence, and isolation. We were living with a disease the system did not acknowledge.
These stories are not isolated—they reflect a silent, systemic failure affecting countless families and children. Their pain and courage are what fuel my fight for an equitable, people-centred health system that doesn't abandon the most vulnerable.
Through experiencing multiple NCDs, I realized the script was the same: late diagnosis, no access to care, lack of medication and treatment, poor awareness, long delays, poor referral pathways. The most affected? Children—who don’t even have a voice to speak out.
During COVID-19, we founded the first cardiac unit in Southern Zimbabwe situated at Mpilo hospital: the second largest hospital in Zimbabwe. This effort came about because children were dying in admissions. During our advocacy efforts, we were told to wait until after COVID-19. But we insisted because these children were at greater risk.
Although the silver lining came, the cardiac unit was not used for its intended purpose. After several follow-ups, we were told: “It’s on government property. It will be used as deemed necessary.” It was repurposed as a COVID-19 isolation unit, while heart patients were placed in infectious wards. More children died. Our spirits were broken. To date, we still hope it will be used for what it was intended for.
We cannot keep building health systems that only respond to what’s visible, popular, or funded by donors. We must build systems that respond to all people, especially those whose illnesses are invisible. No one should suffer in silence from diseases the world chooses not to see.
At Brave Little Hearts, our ongoing work includes collaborating with international NGOs to raise awareness through important days such as World Heart Day and Childhood Heart Disease Week. We contribute to shadow reports that expose inequities in health access. At community level, we provide expert advice on navigating childhood heart disease, peer-to-peer support for parents, hospital and home visits, counselling, food hampers and anti-heart failure medications if available. Additionally, we offer psychosocial counselling for grieving families, and we have plans to expand into agriculture and livestock rearing to support families economically. Our past efforts include petitions to the Ministry of Health, media campaigns highlighting diagnostic gaps, and participating in consultations and technical working groups. We advocate for early diagnosis, decentralized services, and integration of paediatric NCDs into national strategies. We’ve also highlighted how delayed treatment can worsen outcomes during emergencies.
Despite operating without formal funding, we remain committed to making invisible conditions visible, ensuring children with NCDs, especially cardiac conditions, are included in universal health coverage planning.
Becoming a health advocate was never part of my plan. I had no choice. Silence was not an option. It was born out of a deep-seated need to stop history from repeating itself.
1 November 2025
A call from the heart
In my final episode, I share my journey through Zimbabwe’s silent heart disease crisis. I speak as a mother, a caregiver, and an advocate, to raise my calls to action for inclusive, person-centered NCD care before more voices—like my daughter’s—are lost to silence. We demand real inclusion and informed decision-making so that no one is left behind.
Transcript
In this episode, I want to talk about the painful truth of heart disease in Zimbabwe, and how the fragmentation of NCD care—especially in heart health—remains the loudest killer in our communities.
Imagine you are discharged from a hospital, relieved that you have given birth to a healthy baby and then six months later, you are told your child was born with a critical heart condition. It was visible from birth. The signs were all there.
A well-trained medical professional could have picked it up at first glance, but in Zimbabwe, heart patients are invisible. Policies do not name them. Hospitals are not ready for them and countless lives—like my daughter’s, like my parents’—are lost, because heart health and other neglected NCDs remain unseen.
A newborn baby can be discharged with cyanosis and laboured breathing, and no one is held accountable. We are told: “Heart disease often presents late. It is hard to spot at birth.” But what about babies like my daughter who showed clear signs from day one? There was no protocol. No 20-week anomaly scan and no follow-up. Unless you are in a private facility, you are on your own. I was told, “She’s fine, you’re just paranoid.”
Patients suffer neglect, even death, without accountability. When health professionals forget to give oxygen, or the wrong medication is given, or when diagnosis is delayed until it is too late, there is no justice. That has been my journey, my reality and the driving force of why I raise a call from the heart— a call for holistic NCD care, for patient dignity and for inclusion in decision-making and policies.
By the time heart disease is suspected, it is often too late due to poor referral systems. There is no urgency, even for urgent cases. The few machines, such as echocardiograms, are broken or overbooked. Hospitals lack basics such as clean water and electricity, and staff are underpaid and overworked.
If they can afford it, families travel hundreds of kilometres just to be seen, and then they may wait three to six months for a medical report.
The cruelest irony is that even if you get a diagnosis, there is nowhere to go, no emergency fund and no structured help for people needing critical surgery. In Zimbabwe, there is no financial protection for people with heart conditions and care is paid for out of pocket. Every household affected by chronic illness edges closer to poverty. Patients may even be financially exploited in the public system.
Families are left begging on radio stations, posting photos of their babies online, praying that a stranger will step in. Eventually, hope fades and the system forgets your child while you watch them struggle to breathe.
Without inclusion of heart health, the fight against NCDs collapses. We urge policymakers to place heart disease in their NCD strategies.
In Zimbabwe, there is only one practicing pediatric cardiologist in the public sector - yet every year, 4,500 children are born with congenital heart disease and around 3,000 die because they cannot get surgery. Between 2023 and 2025, only 65 heart surgeries were conducted in Zimbabwe among people of all ages. This is a drop in the ocean considering the overall disease burden and reflects the low number of resources attributed to fighting heart disease. Every death is a headline that never gets written. Every week, my phone rings with people asking: “Can you help?” “Where do I go?” “Is there funding?” “Will she make it?”
I have travelled hundreds of kilometres, slept at bus stations, spent money meant to feed my children, just to chase answers and at times have met so much discouragement. I’ve been told: “You’re not a doctor. Do you even have funding? You can’t run a cardiac program, it’s too expensive and uses a lot of resources,” as if the voice and lives of patients and caregivers do not matter.
But my voice, our voice is not only one of grief. It is the voice of survivors who buried countless loved ones, who call for inclusion in decision-making and for policies informed by lived experience FOR people with lived experience.
This crisis is not just about heart disease. It is about the whole health system. Prevention and management of NCDs are crippled by low awareness and scarce resources. Priorities are imbalanced—infectious diseases dominate while NCDs are ignored and excluded from funding models. Government health spending is far below the 15% the WHO recommends. Patient-led advocacy groups like Brave Little Hearts are sidelined due to lack of funds, and unless advocacy is donor-backed, groups like ours are invisible.
We urgently call for:
- Early screening and intervention.
- Functional referral systems.
- Diagnostic tools in every hospital.
- Access to essential medicines.
- Training and retention of specialists.
- Resources and training for community led organisations.
- Training of patient-led organisations to assist with basic checks on other patients, not just for medical personnel.
- Funding for all NCDs—including the rare and neglected, and not just one or two diseases.
- Financial protection for families and a seat for caregivers at the policy-making table.;
- Inclusive policies for children with chronic conditions, including in education, to prevent them being left behind and dropping out of school.
Without people-led networks like NCD Alliance, Global ARCH, and others, the voices of people with lived experience can never be heard and remain silenced.
We have seen small steps with programmes such as PEN-PLUS, but gaps in inclusion and implementation remain. Without including ALL affected communities, commitments are empty promises. Without transparency and accountability, corruption thrives, and lives continue being lost.
NCD Diaries
I seek to support vulnerable families and amplify affected communities' voices in decision-making processes, driving change to ensure better healthcare outcomes for those in need.
Tendai Moyo, lived experience of multiple chronic conditions, Zimbabwe
About NCD DIARIES
The NCD Diaries use rich and immersive multimedia approaches to share lived experiences to drive change, using a public narrative framework.