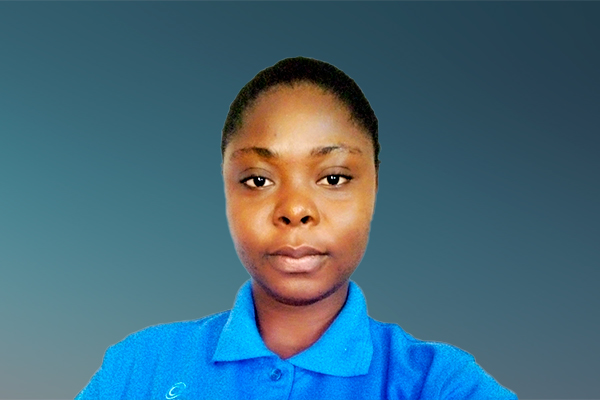
Hi, my name is Wendy and I am from Cudworth, Canada. I have been living with obesity for most of my adult life.
There have been many times that health care professionals have made me feel like my health issues are my own fault because of my weight. This is never okay and I have made it my goal to change how people living with obesity are viewed by medical professionals.
I'm sharing my story because I never want anyone to feel as hopeless, worthless and beat down by healthcare professionals as I have in the past.
12 May 2022
Free healthcare doesn't always come without a cost
Where I live in Canada, you don't have to pay to see a doctor or a specialist. While this is fantastic because everyone has access to treatment, it doesn't always mean that you get treated well. Reflecting on my early journey with healthcare professionals, I feel fear, anger and anxiety. I’ve had interactions with specialists that would make your toes curl, including a statement made by a cardiologist in an emergency room setting. He had no background information on me, didn’t ask questions, and based his “diagnosis” off what he saw in front of him.
“She’s just fat and lazy and doesn’t want to put the work into being healthy.
For many years, this statement had me convinced that because I’m living with obesity, I didn’t have the right to care from medical professionals. I was convinced that nothing could be done and I wasn’t worth saving. I hated myself for letting things get this bad and thought about ending it all just to give those around me some relief from the burden that I imagined I was.
Then one day I visited my family doctor, who had been with us for about a year, to express concern about symptoms I was experiencing that were noticeable in my dad prior to his death from a heart attack. I expected her to say that it was my weight, that I had to eat less and exercise more. I didn’t expect her to sit up and pay attention, and to immediately put in an urgent referral to a cardiologist. But that’s exactly what she did. My low expectations had nothing to do with previous interactions with her, and everything to do with my negative interactions with other healthcare professionals.
Sitting at the cardiologist’s office filled me with anxiety; I was convinced that I was in for another lecture. What happened next would have knocked me over if I wasn’t sitting down. The cardiologist looked me in the eye and explained that my heart was enlarged because I had sleep apnea, so my lungs were lacking oxygen. I’d just started sleep apnea treatment 6 months before seeing him. He was confident that if I continued this treatment, “tweaked my eating and maybe moved around just a little more”, my heart would be fine in under a year. His words saved my life. It’s interactions like these that began to restore my confidence in navigating my care journey, and my faith in the medical profession.
4 July 2022
Shaming and judging are not the way to a solution
“Doctors never talked to me. They either talked at me or talked to my parents about me.
“Because I’m living with obesity, doctors assumed that I had health conditions that I didn’t have.
These statements capture conversations I’ve had with others living with obesity, where we reflected on our journeys – oftentimes since childhood – with healthcare professionals. Through these exchanges I realized the many negative experiences we share. One individual mentioned that they told their doctor they joined Weight Watchers, thinking the doctor would be supportive. What they were told was, “Give me $10 a week and I’ll call and yell at you about what you eat.” Someone else claimed that at the doctor’s office, they could hear the doctor talking to someone at reception about how “fat and lazy” they were. Many others feel they must lie about health-related issues. When it comes time to get on the scale, they’re afraid they will “get in trouble with the doctor.”
Most people claimed that when seeking help from a specialist, they’re often overcome with anxiety and fear. Some are physically ill for days before the actual appointment. I spoke to one person who saw a specialist about her type 2 diabetes. She said the doctor walked in, took one look at her, and told her that she could “cure” her diabetes if she’d stop being lazy and move around anywhere but the kitchen, claiming “food isn’t your friend, and it lives in the kitchen.” Although she said she’d never been an excessively happy person, after she left that appointment, she felt enveloped by darkness. Eventually she tried to take her own life. Luckily, a family member found her and got her to a hospital, and the specialist eventually faced disciplinary action.
Some people feel that they’ve dieted, lost weight and gained it back so often that they wrecked their body. They’re constantly exhausted and depressed. The longer they take to talk to their doctors about what’s going on, the harder it becomes to get through the day. They often feel like they aren’t worth saving. As evidence shows, there is a correlation between lack of quality treatment for obesity and mental health disorders.
Healthcare providers must accept that people living with obesity are not fat and lazy. There are several factors including genetics, medication, and even monetary constraints that can and do contribute to someone becoming obese. There’s a way to discuss obesity-related issues respectfully and helpfully, that doesn’t leave a deflated feeling of failure.
21 July 2022
How do we move forward from here?
Living with obesity is a daily struggle physically and mentally. Not only do we have to live with our shame and self-loathing, but we also must live with the judgement of those around us. Often, we are made to feel that we aren’t deserving of medical help, with many health care providers having been trained to tell us to simply “eat less and move more”. To avoid exhaustion, frustration, and complications that may result from insufficient treatment, people living with obesity must receive quality care from our health care providers.
What is needed is a friendly, accommodating environment for people living with obesity. Not only should medical professionals be trained to effectively and empathetically provide care for people living with NCDs, but also considerations such as larger gowns in doctors’ offices and hospitals can make a world of difference toward helping us maintain our dignity.
On behalf of myself and my community of people living with obesity, I call on health care providers in Canada and beyond to:
- Recognize that obesity is not solely the fault of the person who is living with it. This means that medical professionals need to access the training that is available to them with an open mind and with a people-centered mindset.
- Advocate for people living with obesity to get the best possible care from other doctors and specialists. Speak up if you hear that someone living with obesity has been treated in a disrespectful way. It isn’t always easy, especially in small communities, but it needs to be done.
- When having conversations around obesity, do so with respect. Don’t just lecture the individual about eating less and moving more. While this absolutely works for some people, for some of us it doesn’t, and more help is needed.
- Advocate for more affordable medication and easier access to treatment for people living with obesity. Many people that I have spoken to have said that they would love to try some of the medications that are available, but they are simply too expensive to be affordable long term.
The time for change is now. There needs to be more training available for medical professionals at all levels. There are great strides being made in this direction, but there is still a long way to go.
NCD Diaries
Instead of being ashamed of what you've been through, be proud of where you are now.
Wendy Reaser, lived experience of obesity, Canada
About NCD DIARIES
The NCD Diaries use rich and immersive multimedia approaches to share lived experiences to drive change, using a public narrative framework.