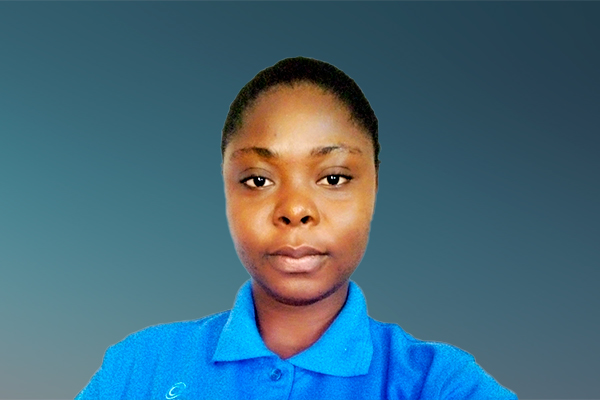
My name is Adjo Rose, I am Togolese and I am 27 years old. I am an office secretary by training, and a volunteer with the Coalition MNT‑Togo.
I am the youngest of a family of eight siblings. Since my early childhood, I did not feel well. I have always had stomach problems, chest aches, headaches and pain in the spine and general and constant fatigue. It really disturbed me in my studies. My father passed away when I was 13. My brothers and sisters have left the house and I am left alone to take care of our mother who is in a bedridden state. This environment has also increased my stress and the lack of financial means prevents me from pinpointing exactly what worsens my condition since sometimes I no longer feel myself.
The tests at the hospital confirmed a gastroenterological condition and I have lived with it ever since. On the other hand, the chest pains, the other symptoms that I feel have still not been officially diagnosed in a health center. I just feel the symptoms.
I write my NCD Diary to convey the importance of affordable, quality, and available diagnostic services to all in Togo. I hope that my experience as well as the experiences of others in a similar situation can inspire policy makers to take urgent action.
17 September 2021
Poverty and chronic pain: I want to get out of it
I am Adjo Rose, I am Togolese and 27 years old.
Since my childhood, I have always had stomach problems, chest pains, headaches, general and constant fatigue as well as spinal pain.
In 2016, tests at the hospital confirmed a gastroenterological condition and I have been living with it ever since. On the other hand, the chest pains, the other symptoms that I feel have still not been officially diagnosed in a health center. Indeed, specialised analyses are expensive, and my financial situation does not allow me to do them. I am forced to make the choice of buying a sedative at a lower cost to relieve my daily pain. I want to put an end to the stress and frustrations associated with consultations and analyses without concrete results.
Despite my state of health, I do not receive any support (psychological, financial, and emotional) from those around me. On the contrary, I have become a subject of mockery because of my regular visits to health centers. This confuses me and slowly draws me into depression.
In Togo, health insurance exists for government officials (INAM insurance) and for those who work in large companies (private insurance) but at a very high cost. The universal health insurance that could help me is only at an embryonic stage (a draft bill was launched in July 2021). Therefore, all the expenses for my health come from my own resources.
In the private hospitals that I go to often, instead of a warm welcome, I tend to be mocked. Indeed no one understands my case and the health professionals I meet say that the origin of my ailments is rather in my head. No one has ever referred me to a psychologist who can only be seen in a private practice or in public hospitals.
I am afraid of public hospitals because I was almost sexually abused by a doctor and yet the specialists who may be able to help me are there. I am working to find a solution to this fear, as in addition to the specialists that work there, from a financial perspective some tests are cheaper in public hospitals compared to private clinics. There also exists an internal social service which supports poor patients.
In my next entry, I will talk about my extended community of people living with NCDs to provide a deeper insight into the infrastructure and affordability of care for NCDs in Togo.
12 October 2021
Vulnerable populations seeking Universal Health Coverage
In Africa, when a situation is unexplained, it is often referred to as a mystery or having spiritual origin. It's the same with health. The solution is prayer or association with traditional deities for those who believe in one or the other.
Often in Togo and African societies at large, people living with NCDs suffer a lack of attention from those around them when they express their symptoms. Not because people don't like them, but because of the chronicity of their ailments, especially if they don't know the origin. They are forced to remain silent, so as not to arouse gossip from others. This prevents them from expressing their need for treatment. Unfortunately, this silence means that no one knows their real needs and that nothing is being done in terms of investment in NCD services.
A training workshop for people living with NCDs in September 2021, organized by the MNT-Togo Coalition as part of the Global Week for Action on NCDs, brought together young people living with different NCDs, in particular type 1 diabetes and respiratory diseases. These young people shared their experiences, including the cost of treatment and inability of their parents or guardians to meet these burdens. For example, a consultation with a specialist doctor in a public hospital in Togo is 3000 FCFA (approximately 5.17 USD) without insurance, and 80% less (1.03 USD) with insurance. In short, insurance covers 80% of hospital costs and 20% is payable by the patient. However, as covered in my previous entry, health insurance is difficult to access for many people in Togo. According to a young uninsured person living with NCDs, his last visit to the hospital cost him 24,600 FCFA (42.38 USD) while he could have paid 4,920 FCFA (8.48 USD) if he was insured. Some have had to leave their families and homes (in remote areas) to consult specialists in town and receive treatment, thanks to charitable associations. This move can impact on their studies and wellbeing. They expressed the relief that access to UHC could bring them, if it is effective in Togo. The discussions during this workshop allowed several participants to learn how to manage, accept and live with their NCD.
Given the costs associated with the treatment of NCDs in Togo, universal health coverage, still in its infancy, seems to be the only way to lighten the financial burden for people living with NCDs. Many will rely heavily on this for lifesaving diagnosis and treatment.
28 January 2022
Situation of People Living with NCDs in Togo: Expected changes
In my previous entries, I discussed my lived experience with NCDs and the difficulties associated with diagnosis, as well as the lack of psychological, financial and emotional support I have experienced from healthcare professionals and those around me. This is largely due to the lack of NCD awareness in my community, which has a significant impact on how conditions are approached and treated, with many people believing that the symptoms of people living with NCDs have mystical origins. I also talked about the Togolese government's plans around implementing Universal Health Coverage (UHC), which many people living with NCDs will greatly benefit from, if this project sees the light of day.
Indeed, this project of the Togolese government is a bill establishing Universal Health Coverage in Togo, which was voted on in the Council of Ministers on 9 September 2021 and unanimously adopted by Parliament on 12 October of the same year. Universal Health Coverage is considered an inception-stage project today, and is expected to become operational in 2030.
Given the timeline (2022-2030) for the full implementation of UHC in Togo, many people living with NCDs will continue to face the financial burden of care for their conditions. There are a number of small support initiatives through certain hospitals, charities and in particular the Coalition MNT Togo in my case, which helps to reduce the financial burden of care for people living with NCDs. However, to accelerate progress, I call on the Togolese government to:
- Reduce the cost of care for people living with NCDs through subsidizing the prices of important drugs and providing free distribution of pharmaceutical products for people living with NCDs.
- Ensure that steps are taken to integrate all NCDs under UHC, effective by 2030.
- Develop partnerships with civil society organizations, particularly those working in the fight against NCDs, in order to meaningfully involve people living with NCDs in the planning and implementation of UHC in Togo.
By implementing the recommendations above, we hope to see that the real needs of all people living with NCDs in Togo are taken into account, and that the financial burden related to NCD care is reduced, even prior to the full implementation of UHC in 2030.
NCD Diaries
As someone who has faced the challenges of an NCD diagnosis, I aim to convey the importance of affordable and high-quality diagnostic services for NCDs in Togo, to ensure that others receive their right to care.
Adjo Rose Lankou, lived experience of multiple chronic conditions, Togo
About NCD DIARIES
The NCD Diaries use rich and immersive multimedia approaches to share lived experiences to drive change, using a public narrative framework.